- 3 min read
What is advanced prostate cancer?
When cancer spreads to other parts of your body, it’s said to metastasise. The cancers that occur elsewhere are called metastases.
Advanced prostate cancer is when the cancer has spread beyond the prostate into other parts of your body. If it has spread into the tissue surrounding the prostate or into the pelvic lymph nodes it is called locally advanced prostate cancer. If it has spread outside of your pelvis to other parts of your body such as bone or distant lymph nodes it is called advanced cancer or metastatic prostate cancer. If you develop advanced cancer sometime after your cancer was treated, it is called recurrent prostate cancer.
How your advanced cancer is treated will depend on the type of cancer you have, its stage and grade.
Prostate cancer stage
The prostate cancer stage describes the size of the cancer and whether it has spread beyond your prostate to other parts of your body. This staging is usually based on imaging scan results.
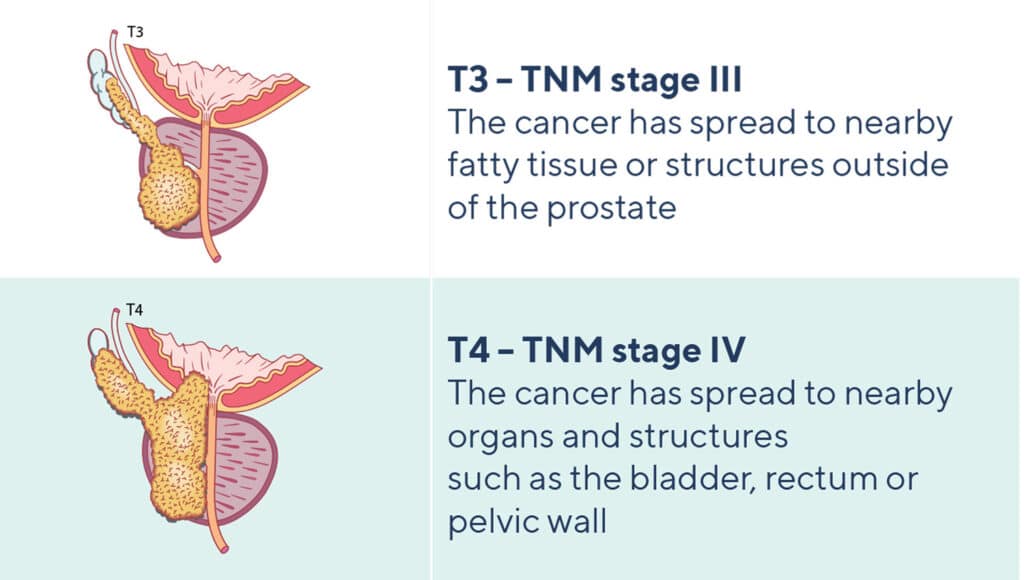
Locally advanced prostate cancer that has spread beyond your prostate will be classified as a stage III or stage IV cancer and may include:
- Seminal vesicles (this is tumour stage T3 – TMN stage III cancer)
- Surrounding organs such as your bladder, rectum or pelvic wall (this is tumour stage T4 – stage IV cancer)
- Spread into lymph nodes in your pelvic region (this is node stage N1 – these are also often called stage III or stage IVa cancers)
Metastatic cancer is when your cancer has spread/metastasised to lymph nodes outside of your pelvis or to bones or other organs – this is metastasis stage M1 and are often referred to as stage IV cancers.
Learn about the tumour and node stages of prostate cancer by following the link to: Stages of Prostate Cancer.
TNM system for determining cancer stage
Localised cancer: TNM stages I or II
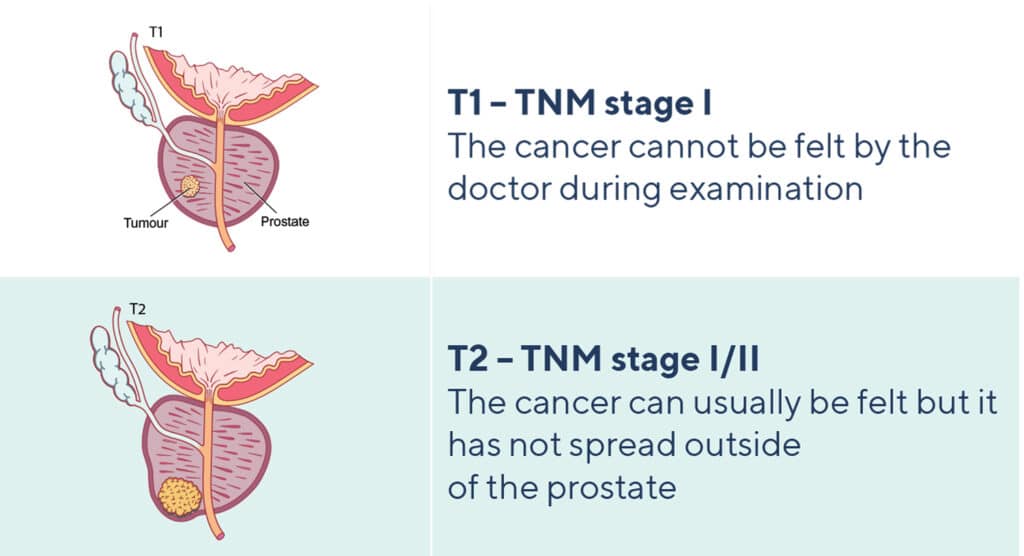
Advanced cancer: TNM stages III or IV
Prostate cancer grade
Prostate cancer grade is determined from a prostate biopsy. This is a surgical procedure where a small amount of your prostate is removed then sent to a pathologist for analysis. If there is cancer present, the pathologist will assign a Gleason score and/or ISUP Grade Group to the cancer. The higher the score or Grade Group, the more likely a cancer is to grow quickly and spread.
Follow the link to learn more about grading prostate cancer: Your Gleason Score & ISUP Grade
Other types of advanced prostate cancer
Most prostate cancers (over 95%) are adenocarcinomas which, if detected early enough, are slow growing with a 5-year survival rate of over 98% (depending on cancer grade and stage at diagnosis). But around 0.2% of prostate cancers are neuroendocrine cancers which are fast growing cancers with a 5-year survival rate of 12%. Neuroendocrine cancers may be detected from a biopsy when you are first diagnosed with prostate cancer or they may develop after you have been treated for prostate cancer.
Another type of advanced prostate cancer is called castration-resistant prostate cancer (CRPC). CRPC is when your prostate cancer cells adapt and grow despite being on hormone therapy and having low testosterone levels. This form of advanced cancer can stay localised to your prostate gland (non-metastatic castration-resistant prostate cancer or nmCRPC) or can spread – this is called metastatic castration-resistant prostate cancer (mCRPC).
Treatments for advanced prostate cancer
Treatment decisions for advanced prostate cancers are based on the type of cancer you have, the extent to which your cancer has spread and where in your body it has spread to. Find out about the different treatments by following the link to: Treatments for Advanced Prostate Cancer
Key Points
- Advanced prostate cancer is when your cancer has spread outside of your prostate gland – it can be locally advanced or metastatic
- Locally advanced is cancer that has spread to nearby lymph nodes and tissues in your pelvis; metastatic cancer is when your cancer has spread to lymph nodes outside of your pelvis or to bones or other organs
- Advanced prostate cancer is staged as Stage III (T3) or Stage IV (T4)
- A biopsy can identify cancer grade and different types of prostate cancer
- Advanced prostate cancer treatments depend on the grade, stage and type of your prostate cancer