- 9 min read
How can prostate cancer treatment affect bladder function and urination?
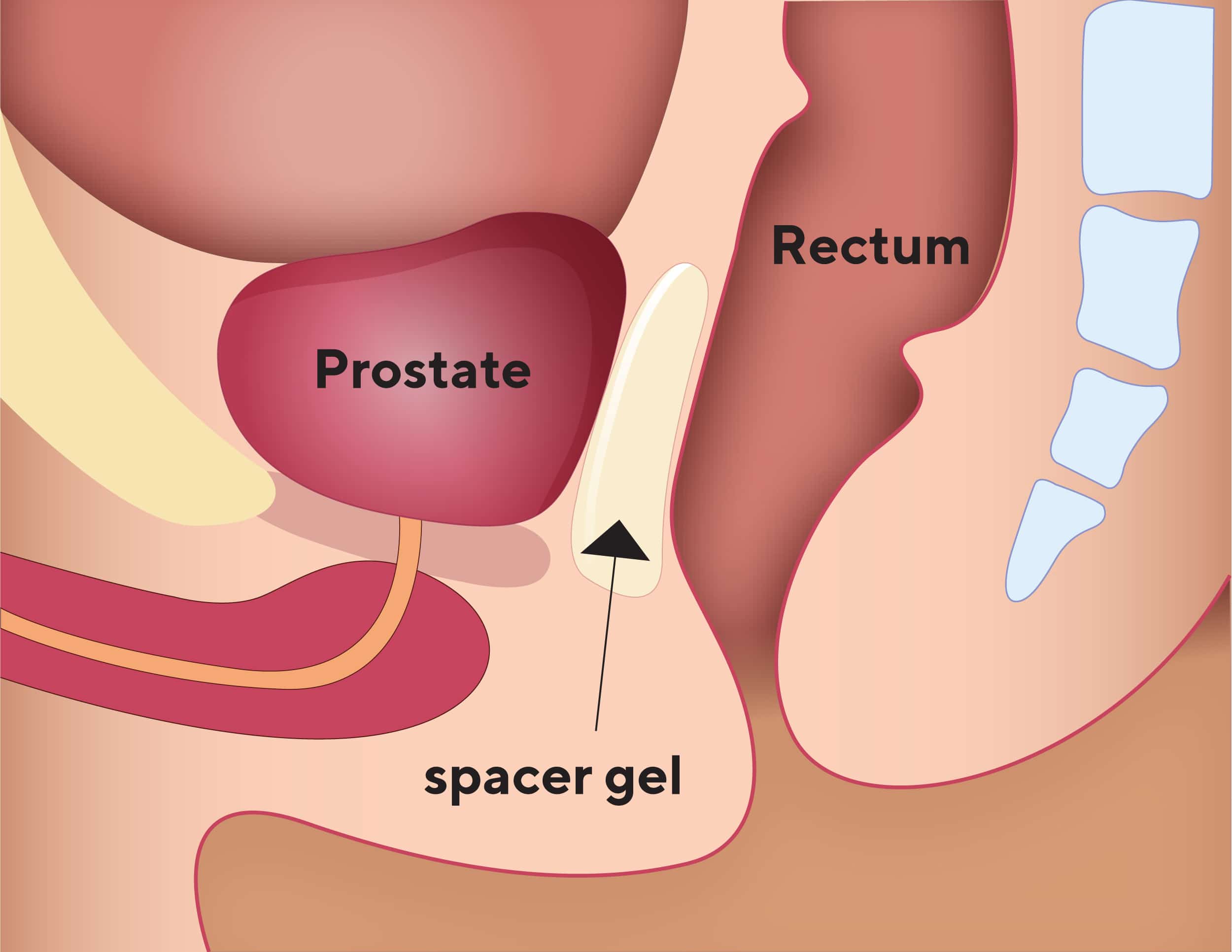
The prostate is a small, walnut-sized gland located below the bladder and in front of the rectum (the lower part of the intestine) in men. It surrounds the urethra, the tube that carries urine from the bladder, and semen, out through the penis.
Problems with urination and your bladder can occur after some prostate cancer treatments, including surgery, radiation therapy and focal therapy.
Follow the links below to see an overview of the side effects that you may experience with or after each specific treatment:
Side effects can happen because your prostate gland sits just below your bladder and treatment may damage or irritate your bladder, urethra, or the muscles and nerves that control when you urinate.
Urinary side effects from prostate cancer treatment can be bothersome and distressing. Often your urinary problems will improve over time but sometimes they don’t go away, and you may need further support and treatment from your healthcare team. You can also reach out to a PCFA nurse if you need advice, support, or more information on treatment side effects.
This section of your toolkit will explain the possible urinary symptoms you may experience after or during treatment and how you can manage them.
What urinary and bladder side effects can you experience after prostate cancer therapy?
The symptoms that you may experience after prostate cancer treatment include:
- Urinary incontinence (leaking of urine)
- Burning or stinging when urinating
- Frequency and urgency to urinate
- Urination flow issues (stop/start or slower stream than usual, difficulty urinating, trouble emptying your bladder)
- Blood in your urine
- Urinary tract infections
If you have blood in your urine, a urinary tract infection or you can’t empty your bladder. Call your doctor, a member of your healthcare team or go to the emergency department.
Urinary incontinence
Urinary incontinence is leaking of urine that you can’t control. It’s a common side effect if you’ve had surgery to remove your prostate but can also occasionally occur after radiation therapy or focal therapy for prostate cancer.
The leakage can vary from an intermittent drop to continual leakage from your bladder. There are several types of urinary incontinence:
Stress urinary incontinence
Loss or leaking of urine when there is an increase in pressure in your belly, for example, when you cough, laugh, sneeze, change position (eg. standing up from a chair) or are physically active
Urge urinary incontinence
Sudden intense need to urinate without the ability to delay it, resulting in the loss or leaking of urine before you reach the toilet – this occurs when your bladder is overactive or contracting without you wanting it to
Mixed incontinence
This is when you have symptoms of both stress and urge urinary incontinence
Overflow incontinence
When your bladder never completely empties, causing urine to leak – this can happen if you have an enlarged prostate, when the bladder and/or urethra is scarred, damaged or narrowed by treatment (sometimes seen in radiation therapy and after surgery) injury or infection
Many factors can contribute to urinary incontinence during or after treatment, including:
Your age
Your weight
Stage of your cancer
Type of treatment
If you were experiencing any urinary problems before treatment
Talk to your doctor or healthcare team about your risk of urinary incontinence after or during treatment, or any symptoms you may have that you’re concerned about. You can also talk to a PCFA nurse.
How do you manage urinary incontinence?
If you’ve had prostate cancer surgery, you will likely have some degree of urinary incontinence after your catheter is removed, about 1 to 2 weeks after the procedure. This is usually manageable and short-lived. Follow the link to learn more about what to expect and how to manage catheter problems.
Urinary incontinence usually improves 1 to 6 months after treatment, but it can last a year or more. A small percentage of men can experience permanent incontinence.
Your incontinence may be managed with:
Continence pads
There is a range of continence products to help you manage urinary incontinence. Supermarkets and pharmacies stock continence products specifically designed for men. You can also buy these products online and get them delivered straight to your home. Some companies provide free samples and sample packs that you can try.
You can try the following:
- Pads are an effective first choice – they are worn with firm-fitting underwear, not boxer shorts, and it’s important to change them regularly and keep your skin clean and dry to avoid irritation
- Bed protectors and containers can be useful if you can’t make it to the toilet in time at night
Ask your GP, healthcare team or a PCFA nurse for advice about different continence products.
Pelvic floor exercises
Pelvic floor exercises are the best way to prevent and reduce urinary incontinence and overactive bladder symptoms (the strong urge to urinate). They can help you regain urinary control sooner after surgery or radiation therapy. You may experience less urine leakage after prostate cancer treatment than men who don’t do these exercises.
After surgery, do not do pelvic floor exercises while your urinary catheter is in place.
Learn about the importance of pelvic floor exercises before and after surgery and radiation therapy and the correct way to activate and strengthen your pelvic floor muscles, with detailed instructions, by following the link to Pre-& Rehabilitation. A physiotherapist or continence nurse can also help you, ask your doctor or healthcare team for a referral.
Other ways to manage incontinence
You may also need certain devices or surgery to manage your incontinence. Follow the link to Pre-& Rehabilitation to find out more.
Burning or stinging when urinating
Radiation therapy can sometimes irritate the lining of your bladder and urethra and cause a burning feeling when you urinate. This usually goes away quite quickly after treatment but can last longer or may develop months or years after treatment.
Burning or stinging can also be caused by an infection, so it’s always important to tell your doctor or healthcare team if you develop these symptoms.
How do you manage burning or stinging when you urinate?
- Drink drinking plenty of water – aim for between 1.5 to 2 litres a day
- Avoid fizzy drinks, tea, coffee, cola and alcohol as these can further irritate the bladder and make you want to pass urine more frequently
- Try drinking cranberry juice, but don’t drink it if you’re taking warfarin or similar medications to thin your blood as it may stop the medications working properly
- Your healthcare team may recommend other drinks you can take can help to make your urine less acidic and reduce the burning or stinging
- Your doctor may also recommend you take medications to relieve your symptoms
- Your doctor may recommend a bladder wash – a procedure where your bladder is filled with a liquid to protect the lining and reduce irritation
Frequency and urgency to urinate
Prostate cancer treatment (radiation therapy and surgery) can leave you needing to urinate more often (urinary frequency), especially at night. You might notice that you suddenly need to go, and you may leak some urine before you make it to the toilet (urinary urgency).
This happens because your bladder muscles spasm and release some urine. Radiation therapy can also scar your bladder tissue causing irritation and a need to urinate more often and/or a feeling or urgency.
How do you manage frequency and urgency to urinate?
A therapy called bladder retraining can be used to help you control your bladder better. Follow the link to Pre-& Rehabilitation to learn more about bladder retraining.
Your doctor may also prescribe medications, a Botox injection in your bladder or a technique that uses a low electrical current to stimulate the nerves that control urination. Talk to a member of your healthcare team or reach out to a PCFA nurse for more information.
It’s also best to avoid drinking large quantities of water or other fluids in the evening to reduce the need for you to go to the toilet.
Urination flow issues
Surgery or radiation therapy can cause a narrowing in the neck of your bladder (where your bladder joins your urethra). This is known as a bladder neck stenosis (or stricture). In surgery this can occur due to scar tissue forming where your urethra was re-joined to your bladder. Follow the link to read what happens during prostate cancer surgery?
Radiation therapy can also scar the tissue in your urethra. This can cause a narrowing of your urethra, called a urethral stricture. This occurs in about 2 to 3% of men and is more common if you have radiation therapy after surgery.
Narrowing of your urethra or bladder neck slows or blocks the urine from flowing from the bladder. This can cause:
- Urinary retention
- Difficulty urinating
- Felling unable to fully empty your bladder
- A weak urinary stream
- Hesitancy
- Spraying of urine when urinating
Urinary retention is more likely if you have an enlarged prostate or if the treatment causes the prostate to swell up. If you develop urinary symptoms after surgery, your urologist may discuss performing a cystoscopy. This is a procedure that involves passing a thin telescope with a camera into your bladder to look at the area and assess if further surgery is required. You may also have difficulty urinating after focal therapy.
How are urination flow issues managed?
There are medicines to treat urinary retention. Sometimes, surgery is needed to widen the opening of your bladder or urethra.
Blood in your urine
Blood in your urine (also called haematuria) can happen after radiation therapy due to scar tissue bleeding. It may also happen immediately after surgery to remove your prostate.
If you suddenly find you can’t urinate or it’s painful, seek medical attention right away. Acute urinary retention can be dangerous. You may need a catheter to empty the urine from your bladder.
It’s often nothing to worry about and clears up quickly, but it’s always important to tell your doctor. You’ll usually be referred to a urologist. They may recommend a cystoscopy and imaging tests.
It’s important to find out the cause of your bleeding as it could be the sign of an infection or another type of cancer.
Sometimes the blood causes clots that can block the flow of urine, so you can’t urinate. If this happens you need to seek urgent medical attention.
How is blood in your urine managed?
Your doctor may adjust your medication to control blood in your urine. Never change your medication yourself without medical advice.
Sometimes treatment for blood in the urine may include using a catheter or a bladder wash. This procedure fills up your bladder with a liquid to try and clear the blood.
If the bleeding doesn’t respond to treatment, your doctor may recommend a special therapy called hyperbaric oxygen therapy, which involves breathing oxygen inside a pressure chamber for 1 to 2 hours. This helps the tissues in your bladder to heal and get stronger.
If the bleeding is caused by cancer or an infection, these will need to be treated by your doctor. If bleeding from scar tissue caused by radiation therapy becomes heavy or prolonged, you may need to have surgery.
Managing side effects and looking after yourself
There are many things you can do to improve and help you manage urinary side effects after prostate cancer treatment. Remember, you can always ask your GP, a PCFA nurse or a member of your healthcare team for advice. You may also find it helpful to talk to others who have experienced side effects from prostate cancer treatments by looking into support groups.
You can download a copy of My Wellbeing Plan to keep track of your appointments, test results and ongoing care information.
Many diet and lifestyle factors can help with bladder side effects, such as quitting smoking, losing weight, managing constipation and exercise. You can find out about healthy eating and exercise through the following links:
For specific rehabilitation therapies before and after treatment follow the link to Pre- & Rehabilitation.
For general tips on recovering after diagnosis, testing and treatment follow the link to Recovery & Rehabilitation.
Key Points
- Prostate cancer treatments, such as surgery, radiation therapy and focal therapy can cause urination and bladder side effects
- Bladder and urination symptoms that you may experience after these treatments include incontinence, frequency, urgency or issues with urination flow
- Many factors can affect urination and bladder function, such as age, weight, cancer stage and type of treatment
- Urinary incontinence after surgery is expected for a short time after your catheter is removed, but it can cause longer term issues with a small number of men experiencing permanent incontinence
- Pelvic floor exercises can reduce urinary incontinence and help you recover continence after surgery exercises
- Some symptoms may also be managed through diet and lifestyle changes, medications, surgery or other procedures
- Always seek medical attention if you can’t urinate, it’s painful or you find blood in your urine