- 19 min read
What is radiation therapy?
Radiation therapy, or radiotherapy, is a safe and effective active treatment for prostate cancer.
Radiation therapy uses either high energy X-ray beams directed at your cancer (called external beam radiotherapy or EBRT) or radioactive material that’s inserted directly into your prostate (called Internal radiation therapy or brachytherapy).
Radiation therapy is a minimally invasive and effective treatment that can be used for localised, locally advanced and advanced prostate cancer
A radiation oncologist will prescribe a radiation treatment plan designed for your unique circumstances. The aim of treatment is to deliver a controlled dose of radiation to your cancer to kill the cancerous cells in your prostate and any that might be in tissues beyond your prostate.
Making the decision to have radiation therapy may feel overwhelming. It’s important to discuss your options with your healthcare team, as they will know your diagnosis and prognosis. They can help you understand if radiation therapy is the right treatment for you.
The aim of this section of your toolkit is to provide you with important information about radiation therapy, the different types, who can have it, and how it may affect you.
Who can have radiation therapy?
Radiation therapy can be given to men of all ages and at any cancer stage.
For localised or locally advanced prostate cancer, it may be offered to you:
- As your main cancer treatment aiming to cure your cancer
- If you are unable to have surgery due to other health issues
- If you have had prostate surgery and need additional treatment – follow the link to read more EBRT after prostate surgery
For advanced (or metastatic) prostate cancer, your healthcare team may offer you radiation therapy to:
- Slow the growth of your cancer
- Reduce pain due to the cancer spreading to your bones – this is called palliative radiation therapy
What are the possible side effects and complications of radiation therapy?
You need urgent medical help if you are unable to pass urine following your radiation therapy
Contact your healthcare team and/or go to your closest hospital emergency department
Radiation therapy, like all prostate cancer treatments, comes with potential side effects, including fatigue and urinary, bowel and sexual problems,. They are often managed effectively, but some can occur many years after treatment has finished.
Radiation treatment will impact your fertility. If you are planning to father a child talk to your healthcare team before starting treatment.
Also, if you have poor urinary function, before treatment, the risk of bothersome urinary problems may increase with radiation therapy. You’ll have a urinary flow test to assess your urinary function before radiotherapy. You may also need surgical intervention to improve any symptoms before starting radiotherapy.
Follow the link to learn more about the side effects of radiation therapy.
How does radiation therapy work?
Radiation therapy works by damaging the DNA in your cancer cells. DNA is the genetic material within cells that they use to divide and grow. When cancer cell DNA is damaged beyond repair, the cancer cells stop dividing and eventually die. It can take several treatments before the DNA is damaged enough for cancer cells to die. For this reason, radiation therapy is often given as a course of treatment over several days or weeks. Radiation therapy is also delivered in two different ways – externally and internally.
What are the different types of radiation therapy?
There are two ways of delivering radiation therapy for prostate cancer:
- External beam radiation therapy (EBRT)
- Internal radiation therapy (also called brachytherapy) – which can also be given as either:
- Low dose rate (LDR)
- High dose rate (HDR)
Not all radiation therapy techniques are suitable for everyone. Ask your radiation oncologist what options are best for you.
External beam radiation therapy – what is it and what does it involve?
External beam radiation therapy (or EBRT) uses a machine called a linear accelerator that directs high energy X-ray beams (radiation) directly at your cancer from outside of your body. When it’s used as the main treatment for your prostate cancer, the radiation beam targets your whole prostate gland, some of your seminal vesicles and sometimes the lymph nodes in your pelvis. It can also be used to treat cancer that has spread to other parts of your body such as bones and lymph nodes outside of you pelvis. EBRT is painless and is like having an X-ray or CT scan.
Generally, you will have this treatment in a radiation therapy centre as a hospital outpatient so you won’t have to stay overnight after treatment. It’s important to note that with EBRT you aren’t radioactive after treatment, and it’s safe to be around people, including children or pregnant women.
You will usually have treatments 5 days a week over 4 to 8 weeks. Most radiation therapy centres don’t open on weekends or public holidays..
Follow the link to find out what happens during an EBRT session
What planning or preparation is needed for EBRT?
There are several preparation and planning steps before your EBRT therapy. This is to make sure your radiation treatment:
- Is as accurate as possible
- Delivers a high dose of radiation directly to your cancer
- Causes minimal damage to the surrounding healthy tissue to reduce the chance of side effects
Planning and preparation helps your healthcare team develop an individual treatment plan for you.
A week or two before your treatment you will have:
- A planning CT scan of your pelvis – this helps your radiation oncologist and healthcare team to see where your prostate and cancer are in your body, so they can plan your treatment and deliver the radiation to that specific area
- The CT scan will take about 15 minutes
- You may be given a few small tattoo dots on the skin of your lower abdomen to help the radiation oncologists make sure you are in the right position each time you have EBRT treatment
Before you have your planning CT scan your radiation oncologist will also let you know if you need any of the following:
- Fiducial marker seeds – your radiation oncologist may advise you to have 3 small gold seeds inserted into your prostate 7 to 10 days before your CT scan
- These seeds show exactly where your prostate is sitting in your body during both planning and treatment, so they can target the prostate more accurately
- Fiducial marker seeds are about the size of a grain of rice and are not radioactive
- They are usually inserted using ultrasound guidance, in a similar technique to a prostate biopsy
- Your radiation oncologist will organise the procedure if you need it
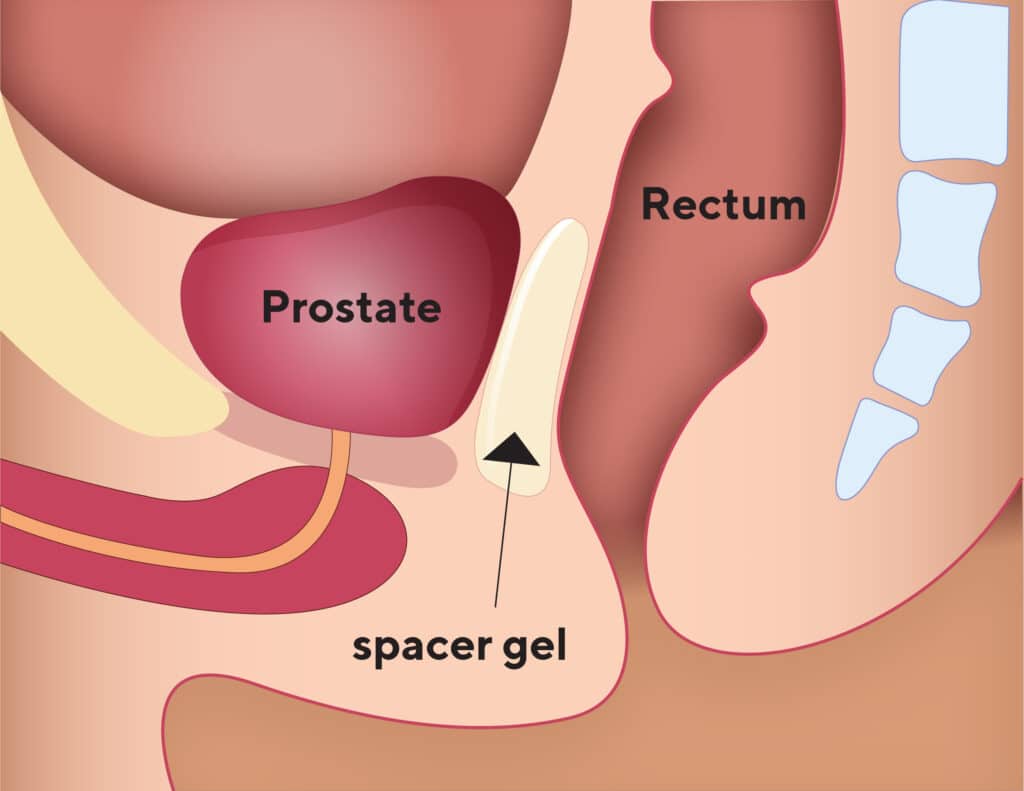
- Prostate-rectum spacers – your radiation oncologist may offer a ‘spacer’
- This is a temporary gel or balloon that’s injected into an area between your prostate and your bowel
- The spacer reduces the radiation to the bowel and lowers the risk of any bowel side effects
- The procedure is usually done as a day procedure with a light anaesthetic
- It’s not commonly available in public hospitals and may not be suitable for everyone
- Magnetic resonance imaging (MRI) – an MRI of your prostate is sometimes recommended to help plan your treatment
- If you need to have MRI it’s often scheduled close to your planning CT scan, so you may be able to have them on the same day
- Bladder and bowel preparation – to keep your prostate in a consistent position
- You usually need to have a comfortably full bladder and to have emptied your bowel before having the CT scan and the EBRT treatment
- Your radiation oncology team will provide you with specific instructions
What happens during an EBRT session?
Your radiation therapy treatment will begin a few weeks after your planning CT scan. This time is used by your radiation oncology team to design an individual EBRT treatment plan for you.
Your treatment visit will usually last around 15 to 30 minutes. Most of this time is spent setting up your treatment so it’s exactly right for you. The radiation treatment itself is relatively short and completely painless.
The steps involved in an EBRT treatment session are:
EBRT is relatively quick and painless and you will most likely be able to return to work, exercise and normal daily activities after treatment
- You will be taken into the treatment room by the radiation therapy team
- The team will position you on the bed in the same way as they did during your planning appointment
- You may feel the couch move a little while you are being positioned
- Before your radiation treatment, a CT-scan, X-ray, or both may be done while you are lying on the treatment bed – these don’t show the cancer cells and aren’t used to monitor how your treatment is going, but ensure your radiation therapy is accurately targeting the correct area
- Often small adjustments may be needed to line everything up correctly for your treatment
- Sometimes the imaging scans show that your bladder or bowel isn’t in the best position, and the treating team may ask you to drink more fluid or open your bowels before treatment is given
- When you are in the correct position, your treating team will leave the room while the radiation beam is switched on, but they will stay in contact with you through TV monitors and an intercom
- You will probably hear the buzz of the machine while it’s working and turning, but you won’t be able to see or feel the radiation beam
Once your treatment is completed, your radiation therapy team will discuss follow-up appointments with you. When you leave the clinic, you will be able to continue with your usual activities for the rest of the day. You will most likely be able to work, drive and exercise as normal. Remember, you aren’t radioactive after treatment, and it’s safe to be around people, including children and pregnant women.
The different modern techniques that may be used during your EBRT treatments
If you have EBRT, your radiation oncologist will most likely use an advanced technique that aims to precisely target your prostate. These include:
Intensity modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT)
In this technique, the linear accelerator machine rotates around your body delivering a radiation beam of varying intensity and shape. This precise targeting of radiation beams around your prostate allows higher doses of radiation therapy to be given safely, while reducing the chance of urinary or bowel side effects.
Image-guided radiation therapy (IGRT)
As the exact position of your prostate will vary a little depending on how full your bladder and bowels are, IGRT involves taking images (X-rays or CT scans) of your prostate area while you are on the treatment bed, but just before treatment is given. These scans are done to check that your prostate (or, if you’ve had surgery, the region around your prostate) matches up with the planning CT scan. This allows the treatment team to adjust where the radiation will be directed before the radiation beam is turned on. It also ensures the radiation is given to the right location every time.
Stereotactic ablative body radiotherapy (SABR), also known as stereotactic body radiation therapy (SBRT)
This is a newer form of EBRT. This technology delivers high doses of radiation to the target area and requires fewer treatments (usually 5 or less). Planning, preparation and side effects for SABR/SBRT are like that for conventional EBRT. However, this technique isn’t suitable for all men, and the long-term results and effectiveness from SABR/SBRT are still being studied. Therefore, it’s not available in all radiation therapy centres around Australia. It may be available through a clinical trial or a centre specialising in the technique. You should discuss your own situation with your radiation oncologist.
Treatment reviews during your EBRT therapy
Between therapy, you will need to attend the clinic several times to see your radiation oncologist, registrar (radiation oncologist in training) and/or a nurse. This is an opportunity to discuss any side effects or concerns you may have.
Hormone therapy may be given with EBRT
Hormone therapy, or androgen deprivation therapy (ADT), are medications often given together with radiation therapy.
Evidence has shown that using hormone therapy before and during radiation therapy can:
- Reduce the chance of your cancer spreading
- Reduce the size of your cancer
- Increase the effectiveness of radiation therapy
- Improve your survival if you have a higher risk cancer
Hormone therapy may be given to you for a short time (4 to 6 months). For higher risk cancers, you may need it for up to 3 years. If required, your radiation oncologist will discuss this therapy and its side effects with you..
Follow the link to learn more about the side effects of hormone therapy.
EBRT after prostate surgery
You may need a course of radiation therapy after you have had surgery to remove the prostate (called a radical prostatectomy).
This option is given to treat prostate cancer cells that may remain behind or that have come back after surgery.
EBRT may be recommended to you after surgery if:
- There were cancer cells found in some of your lymph nodes that were removed from your pelvis at the time of surgery
- Your PSA levels remain detectable after surgery or have started to rise – this is called salvage radiotherapy
- Your PSA levels have been rising after surgery and imaging scans have found an area in your pelvis where the cancer has come back
Radiation therapy given after radical prostatectomy will target the prostate bed (the are your prostate was) and/or the lymph nodes. The prostate bed is the space between the bladder and bowel where the prostate used to be.
There may be a delay before EBRT treatment begins to allow you time to recover from surgery. The planning process and length of treatment for EBRT after a radical prostatectomy is like that for conventional EBRT.
Follow the link to learn more about what planning or preparation is needed for EBRT.
Internal radiation therapy (brachytherapy) – what is it and what does it involve?
Internal radiation therapy (also called brachytherapy) involves radioactive material that is inserted directly into your prostate using special placement needles. Brachytherapy can deliver higher and more precise doses to your prostate and less radiation to surrounding tissues compared to EBRT. The outcome rates and side effects for brachytherapy are similar to advanced EBRT techniques (IMRT and IGRT). However, brachytherapy is not suitable for everyone, ask your doctor if this therapy is a treatment option for you.
What planning or preparation is needed for brachytherapy?
Before having brachytherapy, you will have an ultrasound procedure called a ‘volume study’.
A volume study is done before radiation therapy to:
- Assess the size and position of your prostate
- Provide information on whether your pelvis is suitable to allow the radiation oncologist access to your prostate with the needles containing the radioactive material
The volume study is done as precise measurements of the prostate gland are needed to plan the quantity of radioactive material required and where it will be placed.
How is the volume study done?
The volume study is done in hospital. Your anesthetist may give you sedation or a light general anaesthetic
The volume study involves gently sliding an ultrasound probe into your rectum and taking ultrasound pictures. It takes around 20 minutes. Before the procedure, you may be given laxative medications, a special diet or an enema to clear your bowel. You may also be given some oral antibiotics, in case of infection. You should be able to go home soon after the procedure.
The different forms of brachytherapy
There are two major forms of brachytherapy for prostate cancer. They differ in the type and time the radioactive source remains inside your body, and the rate at which the radiation dose is delivered.
- Permanent low dose rate (LDR) brachytherapy
- Involves a permanent implant of radioactive seeds directly into your prostate
- The radiation only travels a very short distance, so it’s limited to your prostate and a few millimetres around it
- Temporary high dose rate (HDR) brachytherapy
Unlike LDR seeds, the high dose radioactive material is placed into the prostate at the time of treatment and then is removed
Permanent LDR brachytherapy – what does it involve?
LDR brachytherapy is usually used to treat cancer if you have:
- Localised prostate cancer
- An ISUP Grade group of 2 or less (Gleason score of 7 or less)
- A PSA level lower than 10 ng/ml (10 mcg/L)
- Minimal urinary symptoms
However, if you don’t meet these criteria this therapy may still be suitable for you. You can discuss your individual circumstances with your radiation oncologist.
Follow the links to learn more: About the PSA Test, Your Gleason Score and ISUP Grade and Stages of Prostate Cancer
Do I need to go to hospital for LDR brachytherapy?
In LDR brachytherapy, the radioactive seeds are placed in your prostate during a surgical procedure that may take a few hours. You may have the treatment as a ‘day-only patient’ or you may need to stay in hospital overnight.
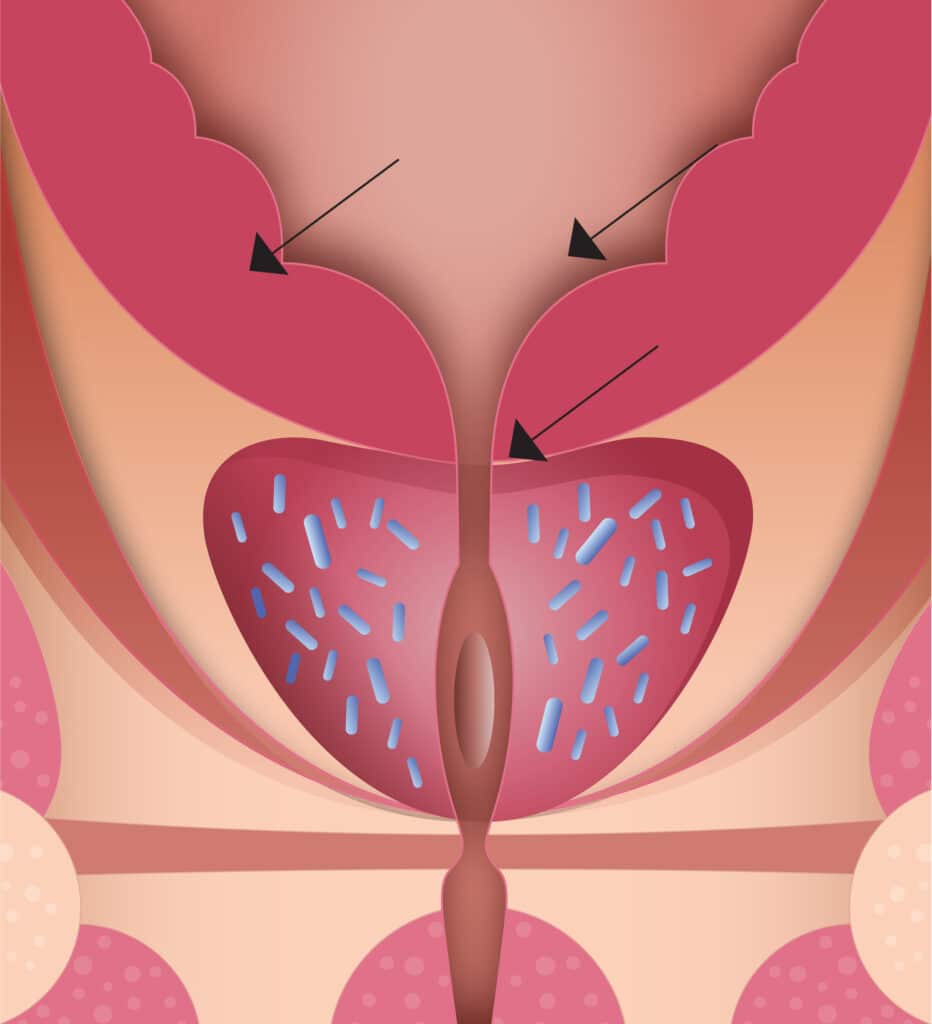
How are the radioactive seeds implanted into your prostate?
Before the procedure you’ll be given either a general anaesthetic or local spinal anaesthetic (epidural). For the procedure:
- The radiation oncologist or urologist will gently insert an ultrasound probe into your rectum so an image of your prostate can then be viewed on a screen
- They’ll then insert 20 to 30 hollow needles through the perineum (skin between your scrotum and anus) into your prostate
- Placement of the needles is guided by a template and the ultrasound images
- From the needles they’ll place approximately 60 to 100 small radioactive seeds into your prostate
LDR internal radiation therapy
Radioactive seeds are placed into your prostate through hollow needles, to kill the cancer cells
You may also have a urinary catheter inserted during the procedure. This is a long thin tube that runs from your bladder through your penis so that your urine can drain into a bag on the outside of your body. The catheter is held in place by a balloon inflated inside your bladder.
What happens after the procedure to implant LDR brachytherapy seeds?
Immediately after surgery, you’ll be moved to a recovery area, while you wake up. In recovery:
- Nurses will monitor your vital signs, including blood pressure, oxygen levels, temperature and heart rate
Once you are stable, you’ll be moved from the recovery area to a hospital ward. In the hospital ward you may:
- Have an ice pack placed between your legs to help reduce swelling to the implant area
- Be given pain relief medications if you need them, although any pain usually settles quickly
- Be given antibiotics to prevent infection and/or medications to avoid constipation
You can usually start eating and drinking once you are awake.
After LDR brachytherapy, what do you need to know about your radiation safety once you have left hospital?
It’s normal for you to be concerned about radiation safety – but it’s important to remember that whilst the seeds are radioactive, most of the radiation is absorbed by your prostate.
Normal social contact won’t put you or anyone around you at risk. Objects that you touch, or encounter, don’t become radioactive. Bodily wastes (urine and stools) aren’t radioactive either.
However, as a precaution, for the first couple of months it’s best to:
- Minimise prolonged contact with babies or young children
- Avoid having small children on your lap for long periods of time
- Avoid prolonged physical contact with pregnant women
- Take certain precautions, like using condoms:
- For some time after the seeds are implanted, for example, for a number of ejaculations or for 1 to 2 months – your healthcare team will advise you
- If your partner is pregnant – ask your doctor if it’s safe to have sex
Your healthcare team will give you specific instructions regarding sexual activity and condom use.
Be aware that your semen may be discoloured for the first few weeks after treatment. Some men also experience some pain with the first few orgasms. This is normal and will get better over time. You can read more about side effects of radiation therapy by following the links to Side Effects and Sexual Function.
What to do if you ‘pass’ any seeds
- It’s rare to pass a seed (through your urine) when you empty your bladder. If you do see a seed in the toilet bowl, flush until it disappears
- If you find a seed in your clothing, use a pair of tweezers to throw it in the toilet bowl and flush until it disappears
Temporary HDR brachytherapy – what does it involve?
HDR brachytherapy may be a treatment option for you if you have intermediate or high-risk prostate cancer.
HDR brachytherapy is usually used to treat cancer if:
- You have locally advanced prostate cancer – disease stage T3
- Your Gleason score is high (the grade of your cancer) or you have larger cancers
Follow the links to learn more: Your Gleason Score and ISUP Grade and Stages of Prostate Cancer
You may also be given hormone therapy or have a course of EBRT before or after your HDR brachytherapy procedure.
What does the procedure for HDR brachytherapy involve?
The procedure for HDR takes place in the radiation therapy department or in a special operating theatre in the hospital. You may have to stay for longer than LDR. Also, unlike LDR, the insertion of radioactive material is temporary. This means that after HDR treatment, there won’t be any radioactive material left inside your body.
Before the procedure you will be given a general anaesthetic. For the procedure:
- The radiation oncologist or urologist will insert an ultrasound probe into your rectum so that an image of your prostate can then be viewed on a screen
- You will also have a urinary catheter inserted
- A template will be placed over the area between your scrotum and your anus
- Implant catheters (or flexible needles) will be inserted through this template
- Placement of the plastic catheters is guided by a template and the ultrasound images
- The number of implant catheters will vary, but there are usually between 15 to 25 implant catheters
- The implant catheters are connected to the machine that delivers the radiation therapy treatment
- Your radiation oncologist or urologist will use a radiotherapy planning scan (ultrasound-based planning technique or CT scan-based planning technique) to determine where the radioactive source should go and for how long
- The radioactive source is passed through the plastic catheters into your prostate
- The treatment itself only lasts a few minutes, but it may be repeated 2 to 4 times while the treatment implant catheters are in place
- You will be transferred to a hospital ward between treatments.
- The template will remain in place along with the implant catheters until the treatment is completed
- When the implant catheters are removed, the radiation treatment is complete
Ultrasound-based planning technique
If the centre where you have this procedure uses an ultrasound planning technique, the placement of the implant catheters, delivery of treatment and removal of the catheters are all done under ultrasound guidance in the operating theatre, while you are asleep under anaesthesia. The procedure takes 2–3 hours and when you wake it will be finished. You may need one or more than one theatre procedures.
CT scan-based planning technique
If you are having treatment in a centre that uses this technique, the catheters are implanted in the prostate while you are asleep under anaesthesia. The catheters are secured in place and X-rays and CT scans are taken to help further planning for your treatment.
In this technique, the implant catheters will still be in place when you wake and you will need to lay flat until they are removed, which may be the same day or the next day.
Keeping flat and still is important as movement may cause the implant catheters to move inside your prostate and this could affect your treatment. If they are bent, the procedure will have to be abandoned. If this happens, alternative options will be discussed by your healthcare team.
What happens after the HDR procedure?
Immediately after the procedure or in between treatments (for CT scan-based planning technique), you will be moved to a recovery area, while you wake up. In recovery:
- Nurses will monitor your vital signs, including blood pressure, oxygen levels, temperature and heart rate
Once you are stable, you will be moved from the recovery area to a hospital ward.
During your stay in hospital:
- You will be given antibiotics to prevent infection
- You can usually start eating and drinking once you are awake, though your diet may be restricted
- You will receive pain relief for the duration of your stay
- You may experience discomfort around the site where the implant catheters were placed – let your healthcare team know about any pain or discomfort and they can arrange medication to help
- Your catheter to drain your urine will stay in place while you are in hospital, and you may have an intravenous drip in place to give you fluids
If you had the ultrasound-based planning technique you may go home the same day. You will be discharged after your urine is clear, your catheter is removed, and you have successfully passed urine. If not, you may need to stay in hospital overnight.
If you had the CT-scan based planning technique, once you have completed your whole course of treatment, the implant catheters, urinary catheter, epidural and intravenous drip will be removed. You will then be discharged when you can pass urine as normal.
It’s important to tell your healthcare team immediately if you are unable to pass urine after these procedures.
After HDR brachytherapy, what do you need to know about your radiation safety when you have left hospital?
Unlike the LDR therapy, after the HDR procedure has been performed and the implant catheters have been removed, there won’t any radioactivity left in your body. You, or any bodily fluids such as urine, won’t be radioactive.
Follow-up care and on-going support after radiation therapy
After completing your course of radiation therapy, you will have ongoing follow up visits with your radiation oncologist to discuss any side effects of treatment you may be experiencing. They will also discuss your PSA test results. You will need to have a PSA test a week before each appointment.
Discussions with your radiation oncologist may include:
- What urinary, bowel or erectile function issues you may be experiencing
- Ongoing management and surveillance based on your individual situation
PSA levels after radiation therapy
After radiation therapy, PSA levels will drop steadily and may take 18 months or more to reach the lowest level – this may be referred to as your nadir PSA level. This means that it may be a few years before you know how successful your treatment has been. If you had hormone therapy at the same time as radiation therapy, your PSA level will drop much faster.
Small rises in PSA levels after radiation therapy does not always mean that your cancer has returned – further testing may be required.
Your specialist may also recommend more PSA tests to check if your levels remain stable, fluctuate or rise. Small rises or fluctuations in the PSA level don’t always indicate that the cancer has returned.
In some men, there can be a ‘PSA bounce’ in the first few years after treatment, where PSA levels temporarily rise and then subsequently fall. This does not mean that your cancer has returned and does not increase the risk of your cancer returning in the future.
If your PSA continues to rise, this usually indicates that you still have prostate cancer cells in your body. Not all men who have a rising PSA will develop prostate cancer that affects their health, and further monitoring may be recommended. Sometimes your specialist will recommend imaging tests, such as MRI, CT and/or PSMA-PET scans, to try to find where the cancer is before they discuss further management options with you.
Follow the links to learn about what the next steps might be for you if your cancer returns – this is called recurrent prostate cancer
Recurrent or Advanced Prostate Cancer
Recurrent Prostate Cancer
Reaching out and being supported before and after radiation therapy
You can download a copy of My Wellbeing Plan to keep track of your appointments, test results and ongoing care information
Having radiation therapy or deciding to have radiation therapy can have physical or emotional effects. Reach out to your partner, friends and family or talk to your doctor or a PCFA nurse. They can connect you with support groups, other health professionals and/or resources for you and your family and friends. You can also contact the Prostate Cancer Counselling Service.
It’s also important to look after yourself before during and after radiation therapy. Follow the links for more information:
Health & Wellbeing provides general tips and information on keeping yourself healthy
Recovery & Rehabilitation for general recovery after diagnosis, testing and treatment
Pre- & Rehabilitation will give you specific advice for before and after treatment
If you are feeling distressed call a PCFA Nurse on 1800 22 00 99 or if you need urgent help, call Lifeline on 13 11 44 or Beyond Blue on 1300 22 46 36
Key points
- Radiation therapy, or radiotherapy, is a safe and effective treatment for any stage of prostate cancer
- Radiation therapy damages the DNA (genetic material) of your cancer cells so they can’t divide and eventually die
- Radiation therapy is delivered to your prostate cancer either:
- Externally through high energy X-ray beams from the outside of your body – this is called external beam radiation therapy or EBRT
- Internally by placing radioactive seeds or material directly into your prostate – this is called internal radiation therapy or brachytherapy
- EBRT requires regular treatments as a hospital outpatient
- You aren’t radioactive after EBRT treatments
- Brachytherapy can be permanent (low dose-rate) or temporary (high dose rate)
- Brachytherapy is done in a hospital under anaesthetic and can deliver more precise doses and less radiation to tissues outside of your prostate, compared to EBRT
- There will be some radiation precautions around social contact for approximately 1–2 months after permanent brachytherapy – there are no precautions with temporary brachytherapy after your treatments
- Outcome rates and side effects are similar between brachytherapy and modern EBRT techniques
- All radiotherapy treatments require planning and some testing before treatment
- You should be able to return to your normal activities, exercise and work after radiation therapy
- PSA levels may take 18 months to drop slowly to their lowest point (nadir PSA level). – this is when you know if radiation therapy has worked, although PSA levels can sometimes temporarily rise and fall a few years after radiation therapy
- If your PSA levels rise consistently after radiation therapy your cancer may have returned (recurrent cancer) and your specialist will further treatment options with you