- 21 min read
What is prostate cancer surgery?
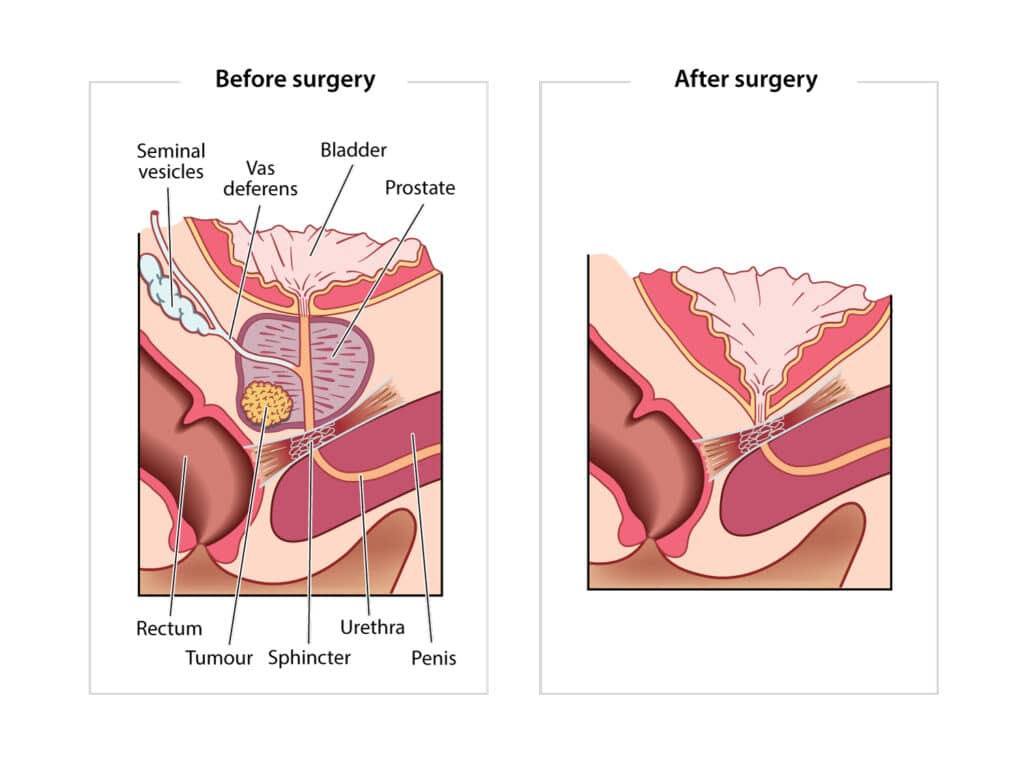
Radical Prostatectomy surgery is a procedure that removes your whole prostate gland.. Seminal vesicles and vas deferens are also routinely removed during a radical prostatectomy.
Surgery is one type of active treatment for prostate cancer treatment, with the aim to remove the entire gland and the cancer and actively treat your disease. It is carried out by a urologist (surgeon) in hospital, and even though you may only have a short stay in hospital, it is considered major surgery.
Making the decision to have surgery can be challenging. Being fully informed will help you decide if this treatment is suitable for you. Ask your urologist plenty of questions or speak to a PCFA Nurse to get a full understanding of the procedure, possible side effects, benefits and costs of treatment.
This section of your toolkit explains prostate cancer surgery, who can have it, how it is performed, and other important information for before, during and after surgery.
Who can have prostate cancer surgery?
You may be offered surgery to treat your cancer if you have:
- Localised or locally advanced prostate cancer that has not spread too far outside of the prostate gland
- Few medical problems or health conditions that may put you at significant risk during or after surgery, including not being significantly overweight
- A life expectancy of 10 years or longer
- Good urinary function
Prostate surgery to remove the whole prostate gland is not usually offered to men with advanced prostate cancer. If you have advanced cancer, still have your prostate and are experiencing issues with your urine flow, your doctor may suggest a transurethral resection of the prostate (TURP). This is a surgical procedure where your doctor will trim any tissue that is blocking your urethra. Sometimes this procedure is offered to men before radiation therapy. Learn more about this procedure by following the link to treatments for advanced prostate cancer.
What happens during prostate cancer surgery?
When you are in surgery your anaesthetist will give you a general anaesthetic to put you to sleep. The operation generally takes between 2 to 4 hours.
You will also have a urinary catheter inserted during the surgery. This is a long thin tube that runs from your bladder through your urethra so that your urine can drain into a bag on the outside of your body. The catheter is held in place by a balloon inflated inside your bladder.
There are 3 different ways your urologist can perform your radical prostatectomy. Your surgeon will choose the technique they have the most expertise in.
1. Open surgery
Your urologist will remove your prostate by making a cut (incision) approximately 8 cm long in your lower abdomen (tummy).
2. Laparoscopic surgery – This is also called keyhole surgery
Your surgeon will make several small cuts in your lower abdomen to insert a small camera and the surgical instruments
3. Robotic-assisted surgery – This is laparoscopic (keyhole) surgery with the help of a robotic system
- This does not mean a robot has replaced your surgeon
- The system has robotic arms that your surgeon will control remotely from a console nearby in the operating theatre
- It gives the surgeon a 3D view of your prostate and your cancer from a computer screen
- Robotic surgery is becoming available in more public and private hospitals around Australia
Is one surgery technique better than the others?
There is evidence sugesting that robotic surgery results in less blood loss and a shorter hospital stay.
Your recovery time may be shorter with laparoscopic or robotic prostate surgery, compared to open surgery – however, all procedures have the same outcome rates and potential side effects.
After making the necessary incisions your surgeon will remove your prostate gland, seminal vesicles and vas deferens, by:
- Cutting your urethra just above and below the prostate
- Moving your bladder down and re-joining it to your urethra
Sometimes, your surgeon will remove the lymph nodes near your prostate to check if the cancer has spread. They may also try to preserve the nerves on one or both sides of the prostate. This is called nerve-sparing surgery.
What is nerve-sparing surgery?
You have nerve bundles running on either side your prostate that affect your ability to have an erection. In a nerve sparing procedure during surgery, your surgeon will try to spare one or both of these nerve bundles, but the ability to do this depends on the extent of your cancer and how far it has spread.
Sparing one nerve bundle is called unilateral nerve sparing; sparing both nerves bundles is called bilateral nerve sparing.
It is important to remember that even if the nerves are spared you may still have some problems with erections after surgery. Ask your surgeon if your nerves were spared, how your erections may be affected, what to expect in the long term and what treatments are available.
What happens to your prostate and other tissues that are removed during surgery?
What happens after surgery when you are still in hospital?
Immediately after surgery, you will be moved to a recovery area while you wake up from the anaesthetic. In recovery:
- Nurses will monitor your vital signs, including blood pressure, oxygen levels, temperature and heart rate
- Nurses will ask you about your pain level and you’ll be given pain relief medications if you need them
- Your urinary catheter, wound drain (if you have one) and wound dressings will be checked
- You’ll be monitored for nausea after the anaesthetic, and be given antinausea medications, if necessary
Once you are stable, you will be moved from the recovery area to a hospital ward.
Your healthcare team will visit you after surgery and let you know when they expect the results from the pathologist. Talk to your surgeon or someone on your healthcare team if you are worried or feel stressed about waiting for the pathology results.
What happens in the days after surgery while in hospital?
Your hospital stay may last from 1 to 5 days, depending on the procedure used and how well you recover.
Your nursing staff and healthcare team will continue managing your care and recovery until you are discharged home. They will help you with any hygiene or pain relief needs immediately after surgery and during your stay. They will also let you know when it is safe for you to eat and drink.
You can also follow the link to Pre & Rehabilitation to find out what else is in involved in rehabilitation after surgery, while in hospital and at home.
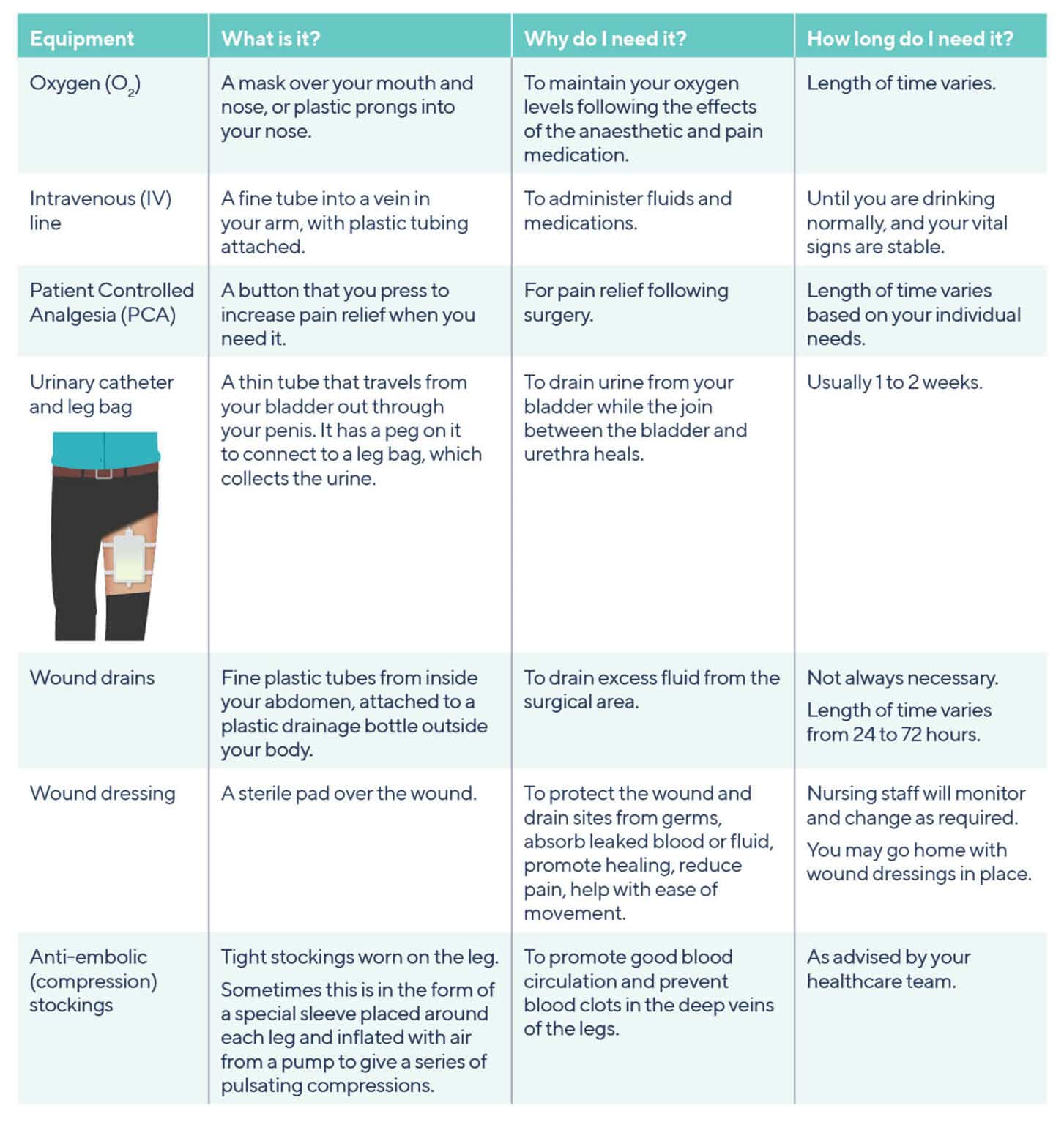
What sort of medical equipment will be used when you are in hospital?
You may be alarmed at the amount of equipment used or around you when you are in hospital. The following is a guide of the equipment you can expect to find. Not all of this will be relevant to you and your individual situation.
How will your pain be managed after surgery?
Your pain levels after surgery will be individual to you. It’s important to ask for pain relief if you need it as it will make you feel more comfortable and help with your wellbeing and recovery.
After surgery you may feel pain:
- In your abdominal wounds– this will significantly improve as each day passes
- From your catheter – you may feel some discomfort from your catheter and have sensations that you need to urinate, but don’t need to go to the toilet
- In your shoulders – occasionally some people feel pain in their shoulders after keyhole surgery
Pain is often measured on a scale from 0 to 10. You may be asked to rate your pain levels using this scale. You are the expert on how much pain you feel. Generally, you will need more pain relief in the first 24 hours following your surgery and will gradually need less and milder forms of pain relief in the following days.
It is important to talk with the nursing staff and your healthcare team about your pain, so they give you the right pain relief or adjust your medication to your needs.
How is pain relief given to you?
Pain relief can be given in a variety of forms while you are in hospital, including:
- Tablets
- Injections
- Patient controlled analgesia (PCA) – this is pain medication that is delivered from a pump into a fine tube in your vein and you press a button to deliver the medication yourself
What are the possible side effects or complications of prostate cancer surgery?
Surgery, like all prostate cancer treatments, comes with potential side effects but also a small risk of complications. Even though your hospital stay may be short, this operation is still considered major surgery. If you are elderly or have medical problems, such as obesity or heart disease, you’ll have an increased risk of complications.
Possible complications of prostate cancer surgery
Your surgeon and anaesthetist will discuss potential complications with you, such as:
Always let your urologist know if you are taking any blood-thinning medications before you have surgery to prevent the rare risk of bleeding during or after surgery.
- A small but rare risk of bleeding or injury to the rectum (the part of the bowel that lies directly behind your prostate) – you should tell your surgeon before surgery if you are taking any medicines to thin your blood, such as aspirin
- A risk of infection
- Blood clots forming in your legs or spreading to your lungs – this complication is rare
Blood clot prevention after surgery
After any surgery, you are at higher risk of having a blood clot in your leg (called a deep vein thrombosis or DVT) or in your lung (called a pulmonary embolism or PE). You are more at risk if you have had a clot previously. Having a DVT or a PE can be very dangerous.
To prevent blood clots forming:
- Your urologist may prescribe medications called anti-coagulants, which are generally given as an injection following your surgery – you may need anti-coagulant injections or tablets at home for a few weeks
- You may be given anti-embolic (compression) stockings to wear just before and after surgery
- You may be asked by your nurse or a medical professional in your healthcare team to walk, sit out of bed, or perform leg exercises while resting in bed or at a chair so you are regularly moving your legs
What are the possible side effects of prostate cancer surgery?
Surgery may cause urinary, lymph gland, bowel and sexual side effects. Constipation is also common after surgery. This may cause you to strain while having a bowel motion, which can affect the healing of the join between your bladder and urethra and your skin wounds. You can follow the link to side effects of treatment to find out what you may experience after surgery.
Most of the side effects can be managed effectively. Your doctor may prescribe laxative medications to help you maintain soft, regular bowel movement after surgery. You can also learn more about looking after yourself and preventing constipation before or after surgery in the Healthy Diet & Lifestyle section of this toolkit. For specific rehabilitation therapies before and after surgery go to Pre- & Rehabilitation.
Benefits and considerations of having surgery
- Surgery is an effective and potentially curative treatment for prostate cancer
- Once the prostate has been removed, the pathologist can provide detailed information about your cancer
- You may take some comfort in knowing that the whole of your prostate gland, including the cancer within it, has been removed
- If you had urinary difficulties due to a narrow or partially blocked urethra before surgery, this treatment may improve these urinary symptoms
- A radical prostatectomy is a major operation and there are risks of complications
- Recovery may take several weeks, and you will need to take time off work and your usual activities
- Prostate cancer may sometimes come back after surgery, especially if the surgeon was unable to remove all the cancer cells. For more information go to the link for follow-up care and on-going support after prostate surgery
What do you need to do or know before surgery?
If you have decided to have surgery to treat your prostate cancer, this section of your toolkit will help you prepare for the operation, know what happens before and during hospital admission, and what happens when your go home afterwards.
How can you prepare your body for surgery?
After your diagnosis, it may be some time before you have your surgery. This allows you time to prepare yourself physically and mentally for surgery. You may feel stressed or anxious about having surgery. Talking with your partner, family or a friend can help. You can also contact the PCFA counselling service.
The Pre-& Rehabilitation and Health & Wellbeing sections of this toolkit provide information on how you can prepare and be healthier and fitter before surgery. This will help you recover after surgery and feel better physically and mentally.
What practical tasks can you organise before surgery?
There are several practical tasks you can do before surgery to make your life easier for when you return home.
- Transport to and from hospital– make sure you have arranged transport to and from hospital as you will be unable to drive for a while after your surgery
- If you live alone it might be helpful to have someone stay with you for a short while as you recover from surgery
Your healthcare team will discuss the removal of your catheter with you before you are discharged. If you are from a country area, you might like to think about finding accommodation close to the hospital. Alternatively, your local community nurse or hospital may be able to remove the catheter. Speak to your surgeon, a member of your healthcare team or call a PCFA nurse on 1800 22 00 99 to get advice about what options may be available to you.
Continence products
You will also likely need to buy some male continence (leakage) pads to have at home for when you first have your catheter removed.
- There are a variety of different men’s pads/shields available – there is no right or wrong choice, and you should use what feels most comfortable and is most effective for you
At home support
Think about what support you will need when you come home from hospital.
- You may wish to organise meals or house cleaning if you don’t have someone to help you at home
Organise leave from work
After the surgery, you will need to take time off work.
- Your urologist will let you know when you can expect to return to work and this usually depends on whether you had open surgery and your type of work, such as:
- Office work – around 2 to 4 weeks leave
- Physical or strenuous work or exercise – around 4 to 6 weeks leave
Complete the downloadable My Wellbeing Plan
Complete the downloadable My Wellbeing Plan, so that you have the contact information for your healthcare team, your surgery date, appointments and other medical information in one handy place, especially for after surgery when you may need to contact a member of your healthcare team for support or advice
You can download a copy of My Wellbeing Plan to keep track of your appointments, test results and ongoing care information.
A social worker can give you information about community services such as cleaning services, meal services and financial assistance. They can also assist you with accommodation advice and arrangements. If your treating hospital does not have a social worker, discuss your concerns with your GP, your healthcare team or call a PCFA nurse for advice on 1800 22 00 99.
What happens before and on the day you are admitted to hospital?
Before being admitted to hospital, your doctor and the hospital where you’ll be having your surgery will give you instructions on what to do before your admission date.
Your doctor will tell you:
- If you need to have any appointments or tests before going to hospital
- If there are any test results that you need to bring with you when you are admitted to hospital
- If there are any special preparations that you need to take before surgery
- What medications you may need to bring with you
- Whether you need to make any changes in how you are taking them
The hospital will contact you to let you know:
- what time and where you need to go when you arrive at the hospital
- when you need to stop eating or drinking before surgery
On the day of your admission, you’ll need to complete hospital admission forms and various doctors, nurses and others in your healthcare team will be looking after you while you are in hospital. They can answer any questions that you have at the time.
What do you need to know about recovering at home?
Before you are discharged and return home, your healthcare team at the hospital will give you instructions on how to look after yourself and who to contact if you have any problems. You’ll also need to make sure you know where and when your catheter will be removed (about 1–2 weeks after surgery) and when you are next scheduled to see your urologist for a follow-up appointment. Your urologist and/or healthcare team will also let you know when you can go back to driving.
Managing your pain at home:
- You’ll be given pain relief tablets to take home
- Follow the instructions your hospital healthcare team give you
- Always ask questions about your pain relief medication if you’re unsure of what to take and when
- As you recover, you’ll be able to reduce the amount of pain relief tablets you take
- You should take the amount of pain relief you need to be able to do normal daily activities comfortably, such as showering yourself, dressing and taking gentle walks
- It’s important to make sure that you take your pain medication regularly as directed, rather than waiting until you are in a lot of pain
Looking after your wounds:
- Before you are discharged, your nurse will explain how to care for your wound before you leave hospital
- Expect to have swelling and bruising around the wounds which will clear up in the weeks after surgery
- Regularly check your wound or the area around your wound dressings for signs of an infection, which include:
- New Tenderness and redness of the skin around the wound
- The area is hot to touch or swollen
- The wound is smelly
- Pus or fluid is leaking from the wound
Contact your GP or another member of your healthcare team immediately if you have any signs of wound infection.
To find out more about general information on rest, physical activity, eating and drinking after treatment go to the Health & Wellbeing section of this toolkit. For specific rehabilitation therapies before and after surgery follow the link to Pre- & Rehabilitation.
How do you look after your catheter care when at home?
You’ll go home with a urinary catheter for 1–2 weeks so the new connection between your bladder and urethra can heal. Before you’re discharged from hospital, you’ll be told how to manage your catheter.
This will include instructions on how to:
- Take care of your leg bag, and how to disconnect it and attach a clean catheter bag
- Change your overnight catheter bag, if needed
- Manage your hygiene needs while you have a catheter
- Secure your catheter to prevent pulling
They will also discuss with you:
- What to do if catheter problems occur – you can also read about troubleshooting your catheter care – what to expect and how to manage catheter problems
- Who to contact and what to do if an emergency occurs with your catheter
- Where and when your catheter is due to be removed
- Information and advice on what to expect when your catheter is removed – follow the link to find out what to expect when your catheter is removed
Catheter
You will have a urinary catheter in place for 1 to 2 weeks after surgery while the new connection between your bladder and urethra heals.
Do not do pelvic floor exercises after surgery while you have the catheter in place. Only do gentle activities while you have a catheter.
Tips on managing your urinary catheter at home
- Drink enough fluids, preferably water, to keep your urine a pale-yellow colour to prevent urinary infection and possible blockage of your catheter
- If you have a medical condition that restricts the amount of fluid you can drink, discuss this with your urologist
- Try to reduce constipation and have regular bowel motions so you don’t strain, as this can cause bleeding. Also, some medications can cause constipation. Talk to your GP if you are experiencing constipation and may need laxative medications
- The Healthy Diet & Lifestyle section of this toolkit also provides general suggestions on how to prevent constipation
- Wash your hands with soap and water before and after any catheter care
- Continue to shower as usual – wash around the head of your penis and under your foreskin (if uncircumcised) in a downward action, at least daily
- Ensure there are no kinks in your catheter or drainage bag
- Keep your drainage bag below the level of your bladder so urine can drain properly and to prevent backwards pressure into the bladder
- Your healthcare team will advise you how to strap or tape the catheter to your leg to prevent pulling, which can cause pressure to the surgical area inside your body
- Wear firm underwear and a pad to help keep the catheter in place
- Empty your catheter bag when it’s half to three quarters full to prevent dragging on the catheter
- Do not do pelvic floor exercises after surgery while you have a catheter
Troubleshooting your catheter care – what to expect and how to manage catheter problems
This section of your toolkit explains what to expect and what to do when you have problems or concerns with your catheter.
What to expect:
Bleeding or leaking urine around the catheter
- It is normal to experience a small amount of bleeding and urine leakage around the catheter (from the tip of your penis)
- This is common when you have had a bowel motion or have lifted something heavy
Discharge around the catheter
- It is also normal to experience small amounts of discharge from around the catheter
- The discharge can be clear/milky and becomes brown when dry
- Gently wash it off in the shower to prevent the tip of your penis from becoming irritated
Bladder spasms and leaking urine
- You may experience occasional spasms in your bladder
- This can give you a feeling of wanting to urinate and is caused by the bladder trying to squeeze out the balloon in your bladder that the catheter is attached to
- Occasionally, this can cause urine to leak around the catheter rather than coming out through the catheter – this is called bypassing
- If the leakage becomes a problem, it can be managed by wearing a small continence pad in your underwear
Blood in the urine
- After your operation, you may notice some blood in your urine
- Drinking water will help flush this out
What to do:
If you are concerned with the amount of blood or discharge around your catheter, leaking urine or are experiencing discomfort or pain with bladder spasms contact your doctor or another member of your healthcare team. If you see blood in your urine for more than 48 hours after surgery, contact a member of your healthcare team.
What do you do if your catheter is blocked or falls out?
Blocked catheter
You need urgent medical help if your catheter remains blocked or has fallen out.
It is important that you tell the doctors at the emergency department that you have had a radical prostatectomy. Ask them to contact your urologist before they do anything, including reinsertion of another catheter.
- It is rare to have a blocked catheter, but if you are experiencing pain in the bladder area or your catheter stops draining urine, check that there are no kinks in the catheter or catheter bag tubing
- Ensure the leg bag is well positioned on your leg and not pulling or dragging.
- Keep drinking water and walk around
- If urine is not draining after following the above instructions, or if you are experiencing pain, contact your healthcare team immediately for further advice or go to the emergency department
Catheter falls out
- If your catheter falls out, contact your urologist, a member of your healthcare team or your treating hospital immediately or go to the emergency department
How to prevent a urinary tract infection when you have a catheter
Urinary catheters can sometimes let bacteria into your bladder and urethra and cause an infection. To prevent a urinary infection, drink enough water to keep your urine a pale-yellow colour (unless you have been advised otherwise by your healthcare team) and keep the area clean where the catheter goes into your penis. Read more tips on managing your urinary catheter at home
Signs of a urinary infection include:
- Cloudy, coloured or smelly urine
- Fever
- Feeling generally unwell
- Pain in the bladder, urethra or kidney area (lower back area)
If you have any of these signs, contact a member of your healthcare team or go to the emergency department. Urinary infections require urgent medical attention.
What to expect when your catheter is removed
You need an appointment with either your urologist or the hospital to have your catheter removed. Make sure you have the date and time for this before you are discharged from hospital, or you know who to contact if you have not received this information. Follow the link for practical tasks you can organise before surgery.
Preparing for the removal of your catheter
Before your catheter is removed you may need to have an X-ray scan called a cystogram. This is an X-ray that uses dye to show the bladder and surrounding area. It is done to check if the area where your bladder and urethra were joined has healed. Your treating hospital and urologist will arrange this for you if necessary.
The cystogram is usually done on the day the catheter is removed, or sometimes the day before. If this scan shows that the join has not healed, then the catheter may need to be kept in for longer to allow more time for the wound can heal and a repeat cystogram test will be needed.
Urination issues after your catheter is removed
Once your catheter is removed, it is very normal to have trouble controlling your urine flow or bladder, so make sure you have continence pads with you. If you have not been given continence pads by your treating hospital, they can be purchased from a supermarket or chemist. Follow the link for practical tasks you can organise before surgery.
Urinary problems or urinary incontinence are often significant in the early weeks after your catheter has been removed, and you may experience leakage all the time.
After your catheter is removed, pelvic floor muscle exercises, done correctly can help you regain control over your urinary flow after surgery
But, with pelvic floor exercises, most men can eventually control their urination and become pad free. This usually occurs within 3 months, but for some it may take up to 12 months. Follow the link to the Pre & Rehabilitation section of this toolkit to learn the correct method for doing pelvic floor exercises, after your catheter has been removed.
After the catheter has been removed and you have returned home, contact your healthcare team or go to the emergency department if you feel like your bladder is full and you are unable to pass urine. For more information read about how surgery may affect bladder function.
Follow-up care and on-going support after prostate surgery
Within the first 4 to 6 weeks following surgery, you should be returning to more of your usual activities. As part of your ongoing care, follow-up appointments will be offered to make sure you are recovering or have recovered from surgery.
You may have your first PSA test and a follow-up appointment with your urologist within the first 6–8 weeks after surgery.
Discussions with your urologist may include:
- How you are recovering from the surgery
- What urinary issues you may be experiencing
- Erectile function and ongoing management based on your individual situation
Your urologist may also discuss the pathology information (stage and grade of your cancer) from your removed prostate and the result of your recent PSA test. They will use these results as a baseline for your ongoing care. Follow the link to learn what happens to your prostate and other tissues that are removed during surgery.
Your urologist will likely recommend more PSA tests to check if your levels remain stable, fluctuate or rise. If your PSA does rise to a certain level, this usually indicates that you still have prostate cancer cells in the body. But not all men who have a rising PSA will develop prostate cancer that affects their health. Further monitoring may be recommended.
Sometimes your doctor will recommend imaging tests, such as MRI, CT and/or PSMA-PET scans, to try to find where the cancer is before they discuss further management options with you.
Follow the links to learn about what the next steps might be for you if your cancer returns – this is called recurrent prostate cancer (or biochemical recurrence).
Reaching out and being supported before and after prostate cancer surgery
If you are feeling distressed call a PCFA nurse on 1800 22 00 99 or if you need urgent help, call Lifeline on 13 11 44 or Beyond Blue on 1300 22 46 36
Having prostate surgery or deciding to have surgery may cause you to feel physically or emotionally challenged. Reach out to your partner, friends and family or talk to your doctor or a PCFA nurse. They can connect you with support groups, other health professionals and/or resources for you and your family and friends. A social worker can give you information about community services such as cleaning services, meal services and financial assistance to help you during your recovery. You can also contact the Prostate Cancer Counselling Service.
It is also important to look after yourself. Follow the links for more information:
Health & Wellbeing provides general tips and information on keeping yourself healthy
Recovery & Rehabilitation for general recovery after diagnosis, testing and treatment
Pre- & Rehabilitation will give you specific advice for before and after surgery
My Wellbeing Plan
You can download a copy of My Wellbeing Plan to keep track of your appointments, test results and ongoing care information
Key points
- Radical Prostatectomy is major surgery which aims to remove the entire prostate gland and the cancer
- Radical Prostatectomy surgery may be offerd to you if have localised or locally advanced prostate cancer that has not spread too far outside of the prostate
- There are 3 different techniques your surgeon can use to remove your prostate and the cancer – they all have the same outcome rates and potential side effect rates
- You will have a urinary catheter put in place during the surgery and will keep it in place for 1 to 2 weeks after surgery
- Prostate surgery takes 2 to 4 hours, you will be in hopsital for 1 to 5 days and it may take you several weeks to recover and return to your usual daily activities
- Your prostate and any other tissue removed during the operation will be analysed by a pathologist who will provide a report stating the stage and grade of your cancer
- You will be given pain relief after surgery and while you are are recovering at home
- There is a small risk of complications after surgery and a number of possible side effects, that could change your bladder, bowel and sexual function
- There are a number of ways you can prepare your body and get organised before surgery – this can help you feel prepared, be fitter and healthier before surgery, and will help with your recovery
- Your healthcare team will provide you with relevant information, instructions and any important contact details so you can take care of yourself and manage your catheter during your recovery at home
- Your follow-up care will involve an appointment with your urologist and a PSA test.
- The pathology and PSA test results will be a baseline for your ongoing care
- If your results and further tests show that your cancer may have returned (recurrent cancer) your specialist will discuss the next best steps with you